Evaluating the impact of testosterone replacement therapy on carotid atherosclerosis: a systematic review and meta-analysis - PubMed
Source : https://pubmed.ncbi.nlm.nih.gov/39183456/
Aim: This meta-analysis investigates the association between testosterone replacement therapy [TRT] and carotid artery atherosclerosis. Methods: 3 databases were searched for studies up to June 2023 per the PRISMA guidelines....
Testosterone therapy shows no association with carotid atherosclerosis or lipid/inflammatory markers, though it raises testosterone levels, suggesting safe use in hypogonadal men without increasing CIMT risk.
Patient Background: A 79-year-old woman presented with persistent hypophosphatemia (serum phosphorus 0.8 mg/dL) and multiple stress fractures involving the ribs, spine, and pelvis, consistent with osteomalacia. Her medical history included type 2 diabetes mellitus, hypertension, obesity, osteoarthritis, and anxiety disorder.
Assessment and Diagnosis: Initial evaluation revealed severe hypophosphatemia (0.8 mg/dL; NR: 2.5–4.5 mg/dL), elevated parathyroid hormone (PTH, 169 pg/mL; NR: 10–65 pg/mL), and normal serum calcium levels. Despite vitamin D supplementation, hypophosphatemia persisted (1.7 mg/dL in 2023), and hypercalcemia developed later (10.9 mg/dL; NR: 8.5–10.2 mg/dL). Renal studies showed phosphate wasting (tubular reabsorption of phosphate [TRP] 56.2%) and elevated fibroblast growth factor 23 (FGF-23, 1694 kRU/L). In 2024, ^18F-fluorocholine PET-CT imaging identified two right parathyroid adenomas, confirming a diagnosis of primary hyperparathyroidism (PHPT).
- How can chronic hypophosphatemia signal early-stage PHPT?
- Why is postoperative monitoring vital in PHPT care?

Does Genotype Affect the Efficacy of PCSK9 Inhibitors in the Treatment of Familial Hypercholesterolemia? - PubMed
Source : https://pubmed.ncbi.nlm.nih.gov/37610687/
Currently, available evidence consistently demonstrates and is in good agreement that, in general, the LDL-C-lowering effect of PCSK9 inhibitors is similar across genotypes, except for compound heterozygous and homozygous familial...
Genetic background slightly affects PCSK9 inhibitors’ LDL-C lowering in familial hypercholesterolemia, with reduced response in compound heterozygous and homozygous cases; clinical factors remain key for management.
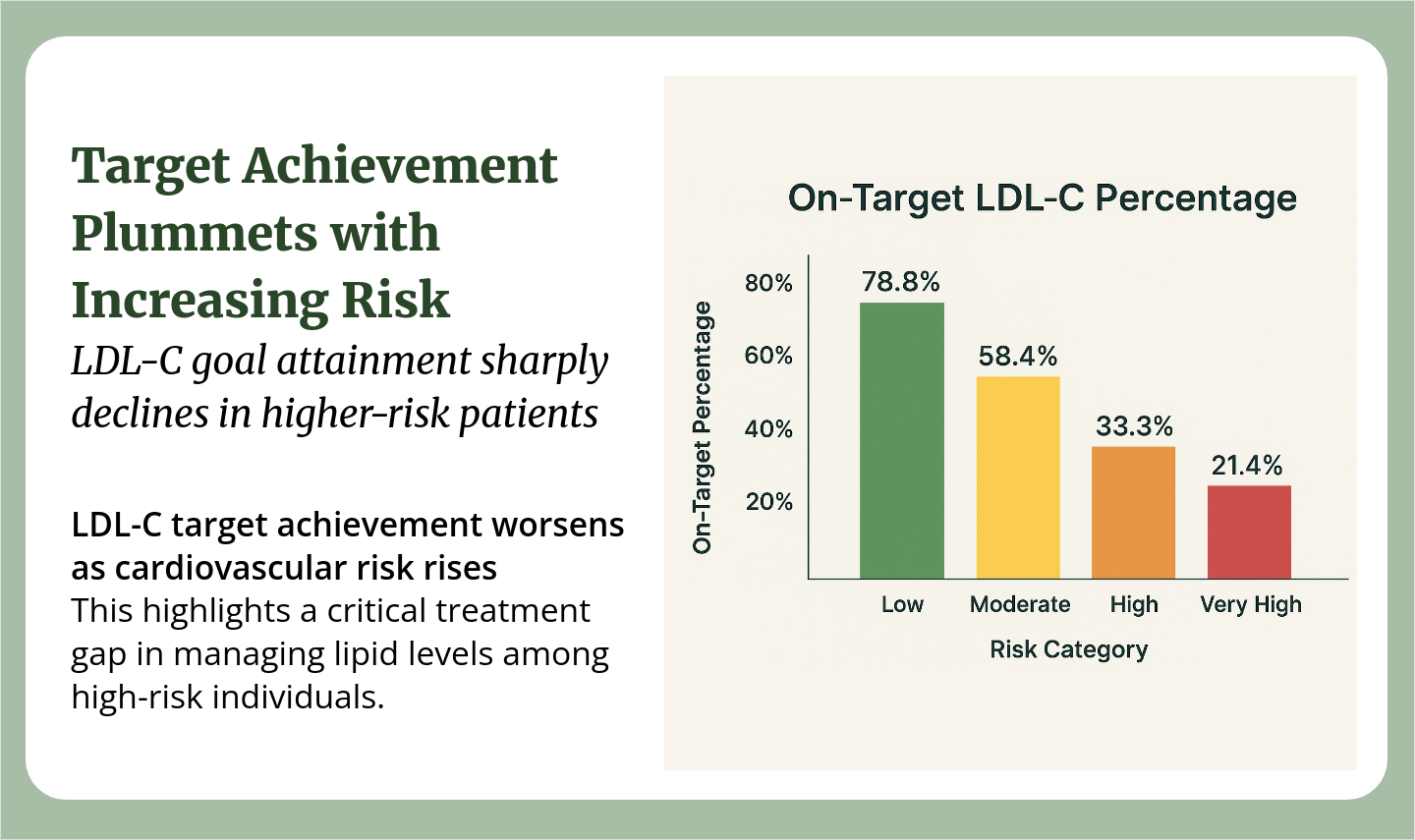
Familial hypercholesterolemia (FH) is often called the “silent accelerant” of cardiovascular risk. From early in life, patients carry LDL-C levels that standard therapy rarely brings to target, resulting in decades of cumulative cholesterol exposure and a significantly elevated risk for premature ASCVD events.
Despite this, FH remains under-recognized—fewer than 1 in 10 patients are ever diagnosed. Missed opportunities for cascade screening and delayed follow-up testing mean many families stay at risk until a major event occurs. Even when FH is identified, achieving LDL-C targets aligned with clinical guidelines remains a challenge.
Clinical data continue to support timely intensification of therapy when conventional approaches fall short. Inhibition of the PCSK9 pathway has been associated with nearly 50% reductions in LDL-C, with added improvements in ApoB and lipoprotein(a). A 2025 meta-analysis showed these effects in both adults and children with FH, reinforcing the importance of early and aggressive intervention in high-risk cases.
Yet real-world care is rarely straightforward. Some patients show a weaker-than-expected response, often linked to missed doses, elevated lipoprotein(a), or genetic variability. Others face barriers tied to access, coverage, or fragmented care, but progress depends on detection, intensification, and follow-up.
How are you identifying FH patients earlier in your practice? When do you escalate therapy—and what has helped sustain LDL-C control long term?
-
 Leon Ronen1moUsually suspect in patients with high LDL, Apo-B, LpA. Perform Dutch lipid score. Usually start statin and watch for response or tolerability. Assess for evidence of CVD - Coronary calcium Show More
Leon Ronen1moUsually suspect in patients with high LDL, Apo-B, LpA. Perform Dutch lipid score. Usually start statin and watch for response or tolerability. Assess for evidence of CVD - Coronary calcium Show More -
 Lana Simmonds1moScreening is performed by routine lipid monitoring. I initiate therapy for those that have FH. If lipid goals are not achieved after follow up lipid evaluation I add on therapy Show More
Lana Simmonds1moScreening is performed by routine lipid monitoring. I initiate therapy for those that have FH. If lipid goals are not achieved after follow up lipid evaluation I add on therapy Show More