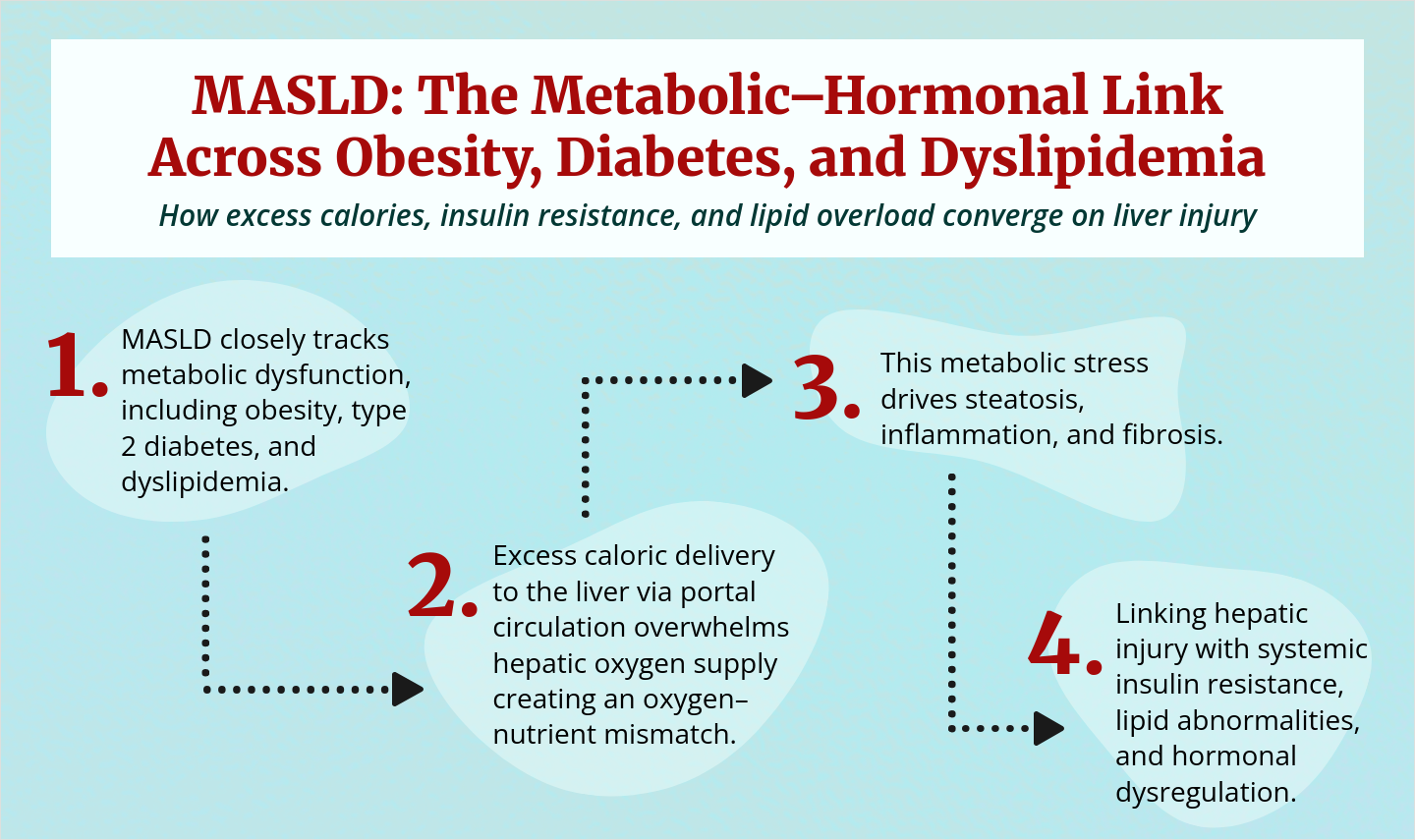
Did you know? Hormonal imbalances can subtly influence lipid metabolism, insulin sensitivity, body weight, and renal function. Disruptions in calcium, vitamin D, and magnesium signaling may amplify cardiometabolic risk, underscoring the need for integrated endocrine monitoring across obesity, diabetes, and lipid disorders to support long-term metabolic health.
Could a more holistic approach to hormonal monitoring improve cardiometabolic outcomes across diverse metabolic conditions?

Could a more holistic approach to hormonal monitoring improve cardiometabolic outcomes across diverse metabolic conditions?