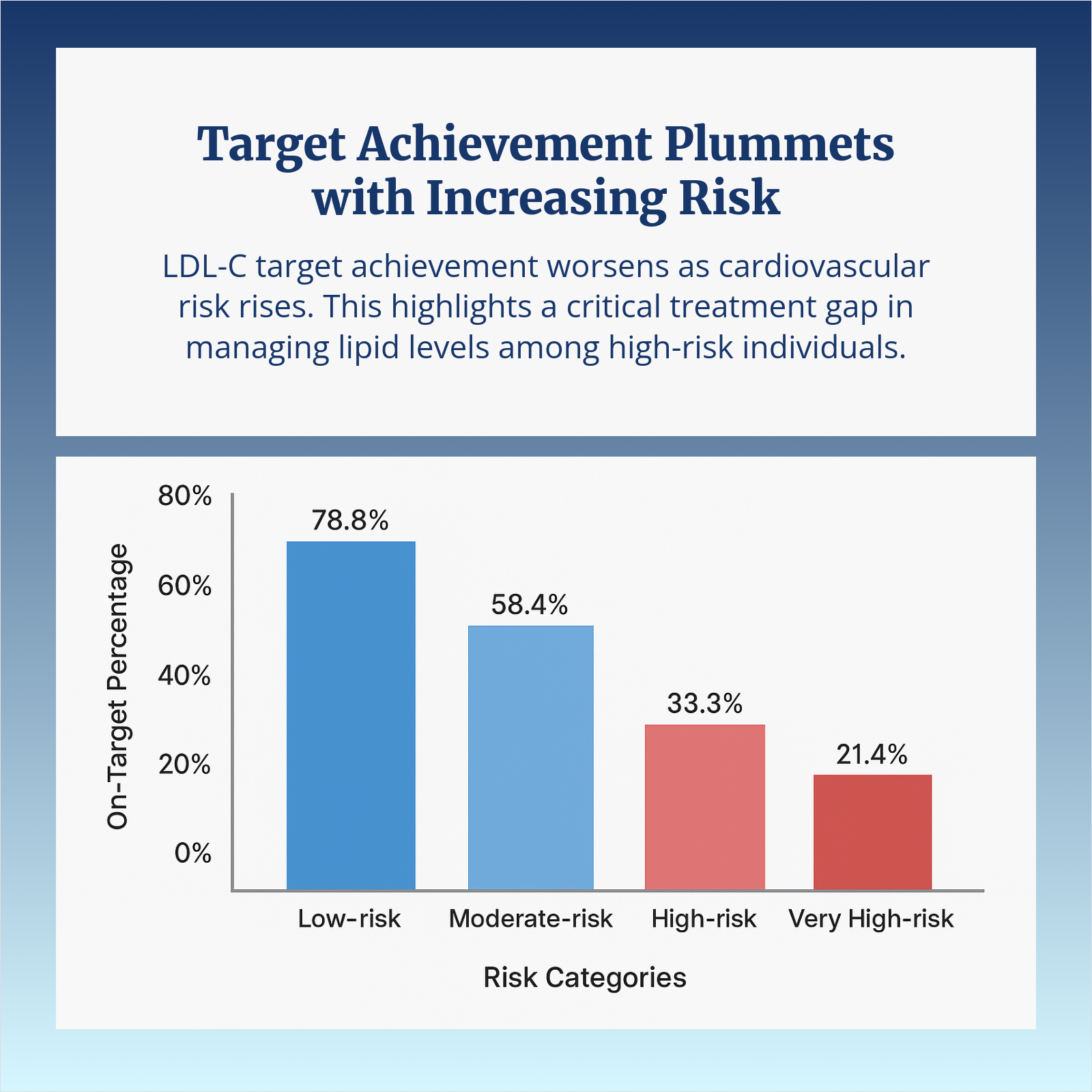
Familial hypercholesterolemia (FH) is often called the “silent accelerant” of cardiovascular risk. From early in life, patients carry LDL-C levels that standard therapy rarely brings to target, resulting in decades of cumulative cholesterol exposure and a significantly elevated risk for premature ASCVD events.
Despite this, FH remains under-recognized—fewer than 1 in 10 patients are ever diagnosed. Missed opportunities for cascade screening and delayed follow-up testing mean many families stay at risk until a major event occurs. Even when FH is identified, achieving LDL-C targets aligned with clinical guidelines remains a challenge.
Clinical data continue to support timely intensification of therapy when conventional approaches fall short. Inhibition of the PCSK9 pathway has been associated with nearly 50% reductions in LDL-C, with added improvements in ApoB and lipoprotein(a). A 2025 meta-analysis showed these effects in both adults and children with FH, reinforcing the importance of early and aggressive intervention in high-risk cases.
Yet real-world care is rarely straightforward. Some patients show a weaker-than-expected response, often linked to missed doses, elevated lipoprotein(a), or genetic variability. Others face barriers tied to access, coverage, or fragmented care, but progress depends on detection, intensification, and follow-up.
How are you identifying FH patients earlier in your practice? When do you escalate therapy—and what has helped sustain LDL-C control long term?
-
 Leon Ronen1hUsually suspect in patients with high LDL, Apo-B, LpA. Perform Dutch lipid score. Usually start statin and watch for response or tolerability. Assess for evidence of CVD - Coronary calcium Show More
Leon Ronen1hUsually suspect in patients with high LDL, Apo-B, LpA. Perform Dutch lipid score. Usually start statin and watch for response or tolerability. Assess for evidence of CVD - Coronary calcium Show More -
 Lana SimmondsYesterdayScreening is performed by routine lipid monitoring. I initiate therapy for those that have FH. If lipid goals are not achieved after follow up lipid evaluation I add on therapy Show More
Lana SimmondsYesterdayScreening is performed by routine lipid monitoring. I initiate therapy for those that have FH. If lipid goals are not achieved after follow up lipid evaluation I add on therapy Show More