Obesity is increasingly recognized not merely as a lifestyle issue, but as a chronic, relapsing disease requiring sustained clinical management. Despite rising prevalence and cardiometabolic risks, pharmacologic treatment remains underutilized. While lifestyle interventions are foundational, maintaining weight loss over time through lifestyle changes alone is often challenging. High-intensity behavioral interventions may yield 5–8% total body weight loss, but this often plateaus or regresses by 12 months.
US clinical guidelines recommend anti-obesity medications when BMI is ≥30 kg/m², or ≥27 kg/m² with comorbidities. However, fewer than 2% of eligible patients receive prescriptions. Barriers such as stigma, limited access to specialists, and coverage restrictions may contribute to low treatment rates. GLP-1 receptor agonists, among newer therapies, address the biological drivers of obesity and have demonstrated significant weight loss (>10–20%) and cardiovascular risk reduction in clinical trials.
With an expanding range of therapeutic options, the focus is shifting to identifying the right patients and aligning treatment with their individual clinical needs and goals. Long-term success often depends not just on initiating therapy, but on sustaining it over time.
What clinical factors guide your decision to initiate pharmacologic therapy for obesity, and how do you approach patient selection, support long-term adherence, and identify those most likely to achieve sustained outcomes?
-
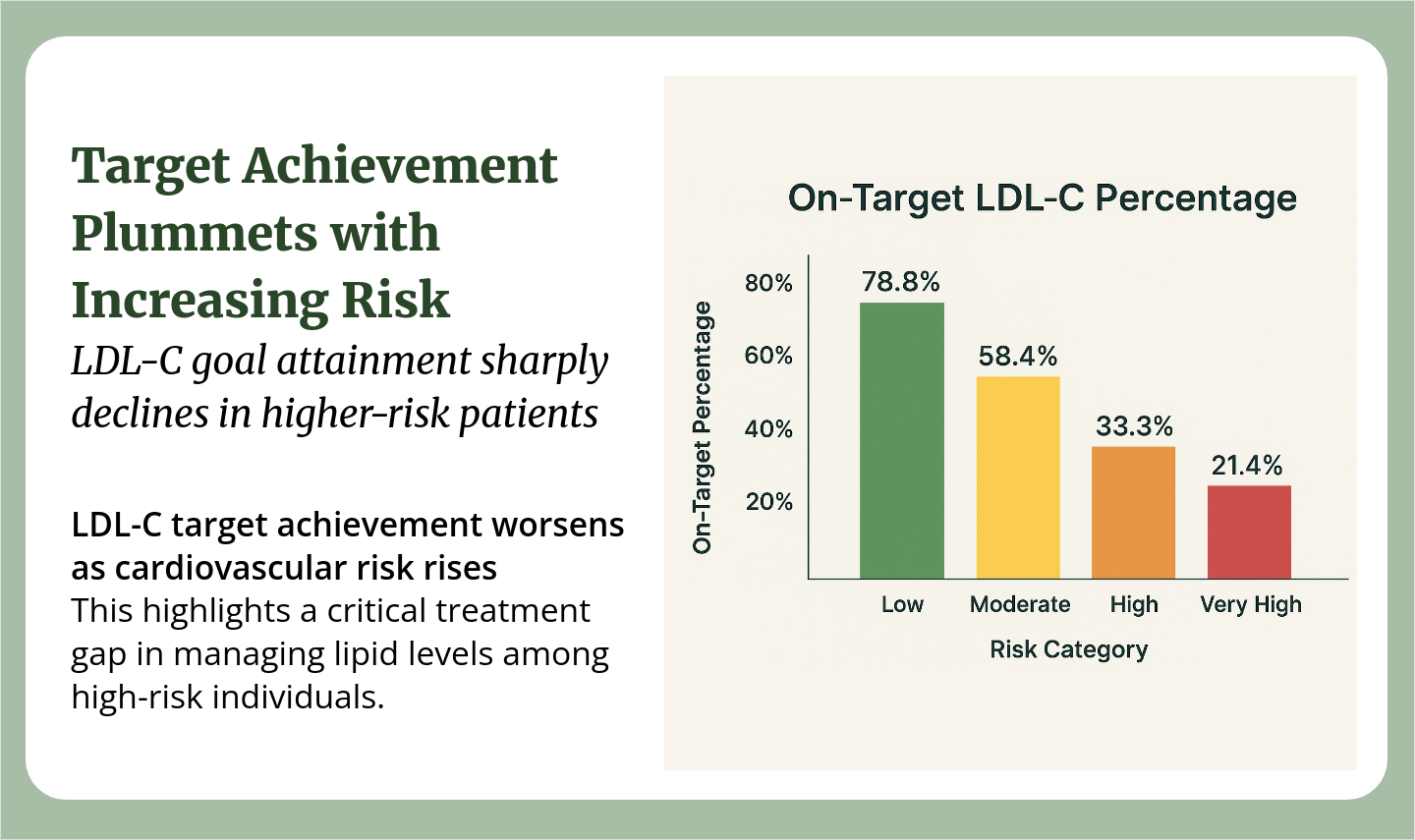
 Sachin Panchal2moPatients with a high burden of obesity-associated disease benefit most: Elevated A1c or prediabetes, Uncontrolled hypertension, Atherogenic dyslipidemia, Evidence of subclinical ASCVD or high 10-yr ASCVD risk
Sachin Panchal2moPatients with a high burden of obesity-associated disease benefit most: Elevated A1c or prediabetes, Uncontrolled hypertension, Atherogenic dyslipidemia, Evidence of subclinical ASCVD or high 10-yr ASCVD risk -
 Peggy Cyr3moI prescribe a lot of weight loss medication. The major barrier is insurance coverage of GLP-1 Agonists. I surprisingly find patients willing to try a once weekly injection. Also once Show More
Peggy Cyr3moI prescribe a lot of weight loss medication. The major barrier is insurance coverage of GLP-1 Agonists. I surprisingly find patients willing to try a once weekly injection. Also once Show More