In 2023, the American Heart Association (AHA) defined a triad of comorbidities—type 2 diabetes mellitus, cardiovascular disease (CVD), and chronic kidney disease (CKD)—as cardiovascular-kidney-metabolic (CKM) syndrome. The AHA identified 4 stages of CKM syndrome as well as a “prestage” of 0 that focuses on prevention and preservation of cardiac health (Table).
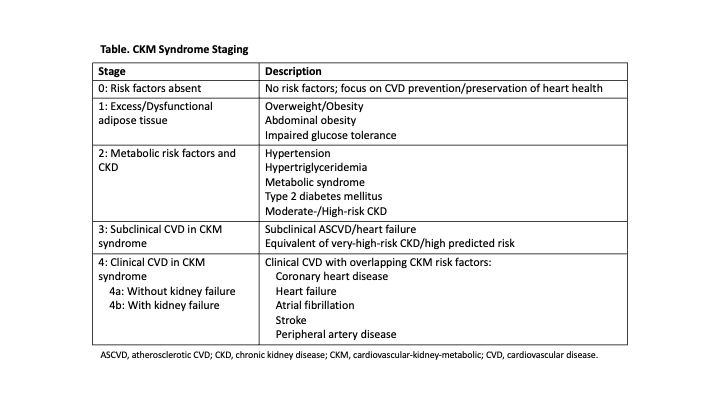
The AHA’s staging model emphasizes the progressive pathophysiology of the disease. It also underscores the importance of early assessment and prevention as cornerstones of patient care—with early detection and interventions often resulting in larger clinical benefit—and it highlights stepwise increases in CVD risk in patients with later stages of the disease.
Several classes of drugs have shown benefit in preventing cardiovascular events, decreasing cardiovascular mortality, and delaying CKD progression. In particular, antidiabetic agents such as sodium-glucose cotransporter 2 inhibitors have cardioprotective effects and can help prevent renal failure.
What protective strategies do you use for your patients at risk for CKM syndrome? How do you facilitate early treatment interventions to avoid disease progression and mitigate the risks of CVD events and kidney failure?


Once patients develop frank disease, the framework is useful for emphasizing how heart disease, diabetes, and kidney disease are interlinked and helping focus attention on therapies (such as SGLT2 inhibitors) that address multiple elements of this triad.
This means weight loss and consideration of GLP1a to assist this for stage 1 patients. Also RAAS, statin, and possibly SGLT2 for stage 2 patients. The onus for early intervention falls on patients via a CKM awareness campaign and PCPs who see patients while they are stage 1 and 2.
The usefulness of this algorithm is that it resensitizes the clinical to the varied risk factors and their interconnectedness.
How aggressive to be is a gestalt for me rather than a stage.
A number of tools we use to treat known CAD, and known CHF, may seem logical to use earlier but may not be studied or approved as preventative care and certainly will not be covered by insurance
there is likely a continuum in this cardio metabolic renal insufficient penumbra, and the the best benefits are probably seen with earlier introduction of GMT.
I speak to all of the patients about their condition and how underlying obesity and the insulin resistance will lead to a myriad of health issues. I encourage increase in daily activity, modification of diet to reduce processed foods and refined sugars/carbs.
Blood work includes usual lipid panel, A1c, BNP, and hs-CRP. I stress the importance of systemic inflammation and its role in disease progression.
Once lifestyle changes have been put into place along with educational sessions and sometimes intensive cardiac rehab, I identify what medications can help.
This usually includes metformin, bupropion, metamucil, ACE, statins, SGLT2i, and now more and more GLP1-RAs.
Identifying family members who are also at risk and implementing a household strategy leads to higher rate of success.
Very tough problem overall for which lots of support and resources will be needed as we move forward.
Early Treatment, when one part of the syndrome develops. Pharmacological therapy (SGLT2i, ACEI/ARB, BP management, DM management, statins) along with lifestyle changes. Would try to not be very intensive with medications early in hopes that lifestyle changes may still change the trajectory of the process
Later treatment, sadly where most of the patients present. It is too late for lifestyle changes to be the only treatment. Intensive medications as listed above.
Inflammation, oxidative stress, insulin resistance, and vascular dysfunction drive the development of metabolic risk factors, progression of kidney disease, which potentiates the heart kidney interactions leading to cardiovascular disease. Metabolic risk factors and chronic kidney disease further predispose to cardiovascular diseases through multiple direct and indirect pathways.
For the protective strategies at the primary prevention level of CKM syndrome, one should recommend:
1. attaining and maintaining ideal CVH linked to decreased CVD.
2. Multilevel school and family-based interventions.
3. Avoiding weight gain/obesity
4. Nonjudgmental weight loss counseling, comprehensive lifestyle intervention, use of incretin analogues (>10% weight loss is associated with lower CVD events) and in advance cases use of bariatric surgery.
For stage 2 CKM patients, each contributing factors should be intervened namely,
1. hypertension (goal 130/80, pharmacotherapy for those with diabetes, CKD, age>65, or ASCVD risk >10%; ACEi/ARB if CKD or diabetes with albuminuria)
2. Hypertriglyceridemia (lifestyle change, statin if intermediate/high ASCVD risk; if diabtetes+triglycerides >135 mg/dl then icosapent ethyl therapy)
3. MetS (lifestyle change/weight loss)
4. Diabetes (statin +/- ezetimibe to achieve 50% LDL reduction, SGLT2inihbitors, GLP-1RA and metformin with SGLT2i if HBA1C >7.5%)
5. CKD (ACEi/ARB in albuminuric CKD, SGLT2i in CKD with GFR>30 ml/min/ , Finerenone in CKD with diabetes with GFR >25 ml/min/ )
The CKM stages 3 and 4 are advanced and treatment is targeted towards the same risk factors with an increasing amount of target organ damage.